Not very tasty. Would not recommend.
Yesterday was The Child’s first day of the new school year. He wore a new shirt, had a new lunchbox and water bottle and we took photos with our chalkboard sign showing his grade. Then I buckled him into the car and watched as my husband drove away with him. I couldn’t go along for the drop-off on his first day of school.
Why not? Because my dad had a doctor’s appointment. I quickly logged on to my computer, checked email while I ate breakfast, fed the cats, fielded a phone call from dad’s nurse, another from my husband describing the school drop-off and ran out the door. I pulled up to my dad’s assisted living facility. I rolled his wheelchair to the car, helped him maneuver his fluid-filled limbs into my Grand Cherokee and wrestled the wheelchair into the trunk. Then I buckled him into the car. His right shoulder, fractured earlier this year, doesn’t allow him the range of motion to do it himself.
We pulled up to the doctor’s office in the pouring rain. I unloaded the wheelchair and helped him back into it. We both got soaked while I pushed him to the door. Thankfully, a kind woman was coming out and held the door for me. I was panting as I checked him in – wheelchairs are heavy.
The doctor was prompt and thorough but concerned. Dad is retaining a lot of fluid. Change the diuretic, do an EKG, get a B12 shot. During the EKG, I checked my email and smiled at the comments on Facebook about The Child’s first day of school pictures. Pushed the wheelchair down the hall for a chest x-ray, then down the hall the other way for an echocardiogram. Maybe Dad has congestive heart failure. Maybe not. We’ll find out in a week or so, says the nice technician. CHF will be a fun add-on to the COPD he already has, plus the abundance of balance and movement issues leftover from a childhood accident. I try not to borrow trouble. We’ll get the results soon.
Take Dad back to the facility. Slide the wheelchair out of the trunk (grab the soccer ball before it rolls away!). Roll him inside, hand the paperwork to the receptionist, hurry back out to move my car so the daughter or son idling behind my Jeep can do the same thing. Notice I missed a call from Mom; she left me a voicemail.
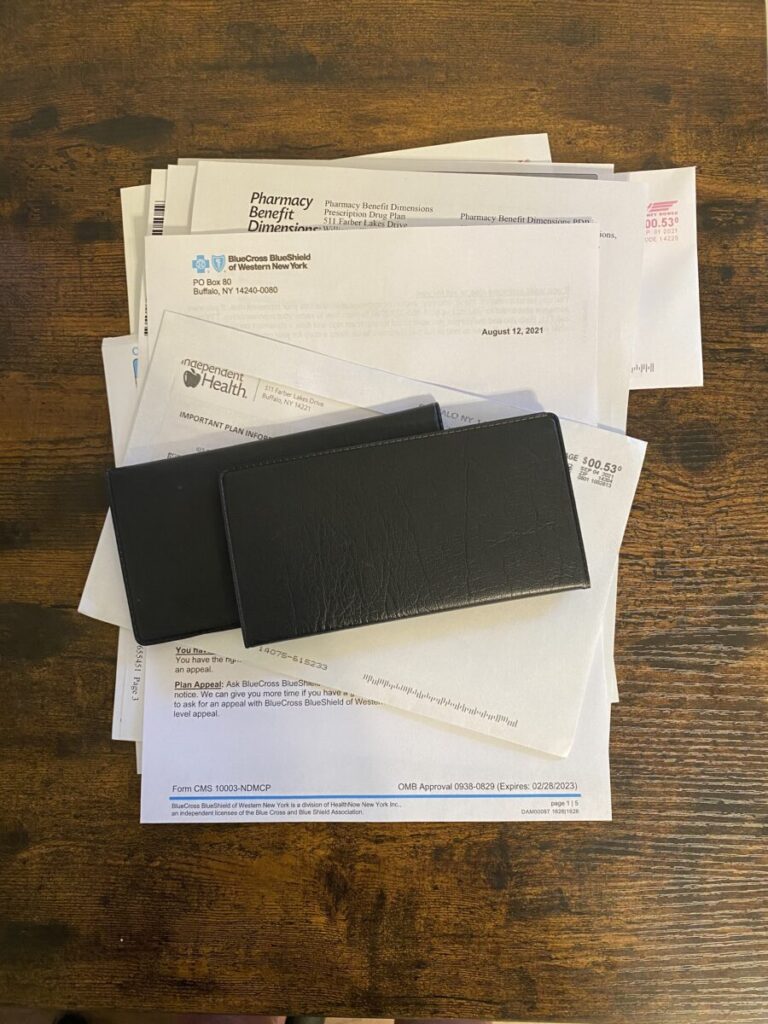
Hustle back home. I had two hours to eat lunch and get some work done before I picked The Child up from school. Then I spent two more hours working and trying to spend time with him before dinner. Today, when I’m not working, I’ll pay bills on behalf of both parents (POA for both of them, thank you very much, and yes, I have HIPAA authorization on file) and sort through the pile of paperwork I get from both of their health insurance companies, Medicare, Social Security and their respective assisted living facilities. (I didn’t have the sense to put them both in the same facility – they’re divorced, so it seemed prudent to separate them.) Maybe I’ll take a walk or do some yoga at lunch, if I have time. In the afternoon, I’ll pick The Child up from school and drive him to tennis practice, where I’ll divide my attention between watching him and working on my laptop.
This week happened to be Dad’s appointments, but sometimes it’s Mom’s. She runs more to diabetes and chronic anxiety. The diabetes took her sight more than fifteen years ago, so she also has balance and movement issues which make it difficult to transport her to appointments. Mom likes to talk on the phone and is more social than Dad. The missed phone call from her earlier was a request to send in some cash so she can join a football pool. She calls again later in the day to make sure I got her message. I let her talk while I work, contributing a “really?” or a “wow” now and then.
I bet many of you can relate. In fact, I bet many of you have it harder. Maybe you have more kids that need your attention. Maybe you have a parent with dementia. Maybe you have a parent who lives with you.
For all my complaining, I am not the primary caregiver for either of my parents. They both live in well-equipped facilities with trained staff who cook their meals, help them bathe and dress and administer their medications. Earlier this spring, when my dad fractured his shoulder and could no longer live alone, he stayed with me for two weeks while we waited for a space to be available at our chosen facility. Those two weeks were the longest of my life. At his best, my dad is a stubborn, grumpy, rude man who likes to eat Hot Pockets and yell at the television while he watches the local news five or six times a day. He was not at his best. It was very stressful for all of us. He needed far more care than we could provide, and it was difficult to get any home health staff to come in to care for him for such a short time. We were all relieved when he was able to move into the facility.

For those of you who are caring for loved ones in your home, I salute you. It is a hard, hard thing to do, and whether you do it out of love or out of obligation, you are doing it and it is no small thing. Whether or not your loved ones live with you, caregiving is tough. 1 out of every 5 American adults is a caregiver, and most caregivers are between the ages of 50-64. If you’re caring for both children still living at home and aging parents, you fall into the “caregiver sandwich.” I am smushed solidly in the middle of the sandwich and I’m not alone. 44% of Americans ages 44-55 have at least one parent still living and at least one child who is under age 21.
The “caregiver sandwich” comes not with fries or a pickle, but with a large side order of guilt. Guilt for neglecting your children to tend to your parents, or vice versa. Guilt for not being a better parent or a better son/daughter or a better employee or a better spouse (or any combination of those things). Guilt for being angry with your parent for getting older or frailer or sicker. Guilt for taking time to do anything for yourself – a haircut, a vacation, a mammogram. Guilt when your spouse or child is completely understanding about a disappointment, as in, “It’s ok, Mama, I understand you can’t go on my field trip because someone needs to stay home with Grandpa.” Guilt, guilt, guilt. You will pile it onto yourself, but rest assured, you will get plenty of it from the outside world as well. There is no shortage of it.
I have known many caregivers during my career and during my personal life and have seen the toll it takes on them. Caregiving can be rewarding and satisfying and many caregivers report that their relationships with their loved ones are deeper and more intimate as a result. However, caregiver stress is real. Many caregivers sacrifice their own health and relationships to care for their loved ones. Studies have shown that caregiving can lead to deterioration in physical, mental and emotional health. Caregiving has been linked to weakened immune systems, obesity, increased risk for chronic diseases and problems with short-term memory and focusing. As many as 40-70% of family caregivers have clinically significant symptoms of depression.
It’s easy to recommend self-care, or taking a break, or “finding time for yourself.” It’s harder to make it happen. Here are some ideas that have worked for me.
Ask for help from people who have been there.
Who better to ask for caregiving help than people who have done it before? Seek out the people in your life who have cared for their loved ones and know what you’re going through. Just like seasoned parents know that a first-time mom needs someone to hold her baby for an hour so she can take a shower by herself, seasoned caregivers know how to help. When my dad stayed with us, my husband and I needed to tend to some chores together, but we needed a sitter – for both The Child and my dad, neither of whom could be left unsupervised. I reached out to a friend who had been the primary caregiver for her husband for almost two years before he died. She came over and “babysat” for both of them – made lunch and played with The Child and helped my dad to the bathroom without batting an eye. You can’t beat the experience of a seasoned caregiver
Be very specific about what you need.
Just like when you have a new baby or a death in the family, people want to help, but don’t know how. If someone says, “Is there anything I can do to help?”, delegate and give them something specific to do. Can they run to the grocery store for you? Take your kids to the movies? Bring you a meal? Sit with your parent for an hour so you can take a shower? Ask for what you need. If you don’t ask, the answer is always no.
Find the chunks of time where you can “take a break.”
It might be hard to fit in a yoga class or a long bath, so look for the small chunks of time that are available to you. When your parents and kids are occupied and safe, spend that time doing something for yourself. Dad’s echocardiogram took half an hour. He was safe with the technician. There was no information I needed to jot down. I didn’t need to be there. It wasn’t a huge chunk of time, but it was long enough to read a few chapters, take a short walk or even sit in the car and close my eyes. It’s not much, but it’s better than nothing. It’s the caregiver version of “sleep when the baby sleeps.”
I hope these tips give you some new ideas. If you need more detailed help, contact me to set up a coaching session. We can meet virtually and I will understand if you need to take a minute to get someone a snack or take someone to the bathroom. We can brainstorm ideas, resources and other ways to help you better manage all of your roles – parent, child and caregiver.
Thanks for being with me on this wellness journey.


Leave a Reply